Health students get lesson in teamwork to improve patient care
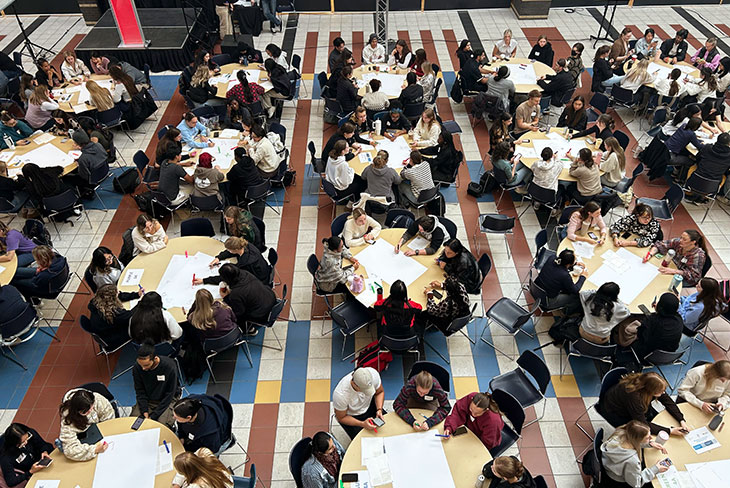
Hundreds of students from SAIT’s School of Health and Public Safety (HPS) joined nursing students from Medicine Hat College (MHC) and the University of Calgary (UCalgary) for a team-building journey through the health-care system at the annual Health Professions Fair.
During the event, students studying a variety of health professions explored the different but complementary roles of the health-care team as they reflected on simulated case presentations inspired by real-life patient stories.
“Health care is about teamwork,” says Jennifer Stefura, Supervisor, Quality and Strategic Initiatives, School of Health and Public Safety. “It’s about understanding how each member of the team, including the patient, needs to work together to support safety and quality of care.”
Attending both in person at SAIT and online, about 750 students from 17 SAIT programs — ranging from Advanced Care Paramedic and Dental Assistant to Health Information Management and Respiratory Therapy — and around 350 MHC and UCalgary nursing students took part.
One of two large interprofessional education (IPE) events undertaken by HPS each year, the fair was presented in partnership by the three post-secondary institutions as members of the Calgary Interprofessional Collaborative Education Committee.
Learning with, from and about each other
IPE is defined as two or more professions learning with, from and about each other and is critical for all health-care professional education programs.
“Our medical system is siloed in how we train people and also in how we treat people,” says Stefura. “We need different perspectives from different health professionals to help us see the bigger picture.”
IPE events aim to build shared knowledge and understanding between post-secondary institutions and diverse professional programs to support a team-based model of health-care delivery.
Team-based care is defined within Alberta’s Health Workforce Strategy as, “a model where interdisciplinary professionals (along with patients and their caregivers) work together to meet a patient’s medical needs and promote/enable their physical, mental, spiritual, and emotional well-being.”
“Many different health-care professions contribute to a patient’s journey through the system,” says Jawad Ali Hashim, Research and Simulation Lead, School of Health and Public Safety. “Some are visible, interacting directly with the patient, while others are in the background.”
Whether they’re up front or behind the scenes, their work and expertise are critical to the overall care of the patient, he says.
“If the wrong information is entered into the computer when creating a patient record, it can put the patient at risk. If I have surgery and I’m not getting a properly sterilized instrument kit, that can derail everything.
“We want this to trigger in the students’ minds now, when they’re in the early stage of their career.”

Communication is care
The opportunity to practice core capabilities or durable skills, including communication, critical thinking and collaboration, is central to any IPE event.
“Durable skills are foundational — they apply to every job in every discipline in all industries,” says Stefura. “In health care, more patients are harmed by incompetence in collaborative skills and communication breakdowns than by incompetence in technical skills. That’s why team-based training is so important.”
The students attended four unique case presentations. Each presentation kicked off with a simulated patient sharing their story. Faculty and facilitators representing the health professions involved in the case then explained their role in the patient’s care. Some cases featured half a dozen different professional roles.
“The emphasis on patient care had the biggest impact on me,” says Ava Gallup, first-year Nuclear Medicine Technology student at SAIT. “After the patient shared their story, I liked how the health-care professionals told us what they did for the patient, not just what they do as their job.”
Following the presentations the students worked in mixed-member teams to discuss, evaluate and reflect on the case.
“I learned more than I expected from meeting with the other students,” says Gallup. “We’re all part of a large and diverse field, but my group agreed we’re all here due to our passion for helping people.”
Classmate Sydney Krasinkiewicz agrees. “We all care about creating the most positive experience possible for the patient,” she says. “Even though our means of caring and helping may be different, we all have the same end goal.”
Krasinkiewicz also discovered a profession she didn’t know existed: medical device reprocessing technician.
“I still have a lot to learn about the other health professions.”
For UCalgary Nursing student Genevieve Comb, the day offered a powerful new perspective on what it means to be part of a multidisciplinary team.
“Most people think nurses and doctors make up the whole medical team, which isn’t true,” she says. “It was really cool to see how all the jobs intertwined and supported one another.”
From confidence to responsibility
The overall experience is also designed to build confidence. One of the key lessons organizers hope the students take away is that every member of the health-care team is responsible for advocating for the patient and reducing cracks in the system.
“Each profession has its domain — in your domain, you’re the expert,” says Ali Hashim. “Part of your role working on a health care team is to give feedback and direction based on your expertise. If you see something happening that puts the patient’s safety at stake, you need to speak up.”
Although there can be lots of overlap between skills and scope within the professions, decision making in health care is often hierarchical, explains Stefura. But the more you know about everyone’s role on the team, the more you respect and value each perspective on what’s happening — including your own.
“Teamwork is obvious during a code,” she says. “Everyone in the room is working on the patient together in the moment. It’s common in that situation for the lead to stop and ask, ‘what am I missing?’ and that can make it easy to speak up. But communication can get more challenging between the team members over time, which is when disconnects can happen.
“These events are trying to get the students to see more broadly into the health-care team and the health-care system,” says Stefura. “Patients don’t just show up in a single moment. They’re on a path. We want our grads to help connect all the pieces of the patient journey.”


Oki, Âba wathtech, Danit'ada, Tawnshi, Hello.
SAIT is located on the traditional territories of the Niitsitapi (Blackfoot) and the people of Treaty 7 which includes the Siksika, the Piikani, the Kainai, the Tsuut’ina and the Îyârhe Nakoda of Bearspaw, Chiniki and Goodstoney.
We are situated in an area the Blackfoot tribes traditionally called Moh’kinsstis, where the Bow River meets the Elbow River. We now call it the city of Calgary, which is also home to the Métis Nation of Alberta.